What is Defination of Rheumatoid arthritis ?
Rheumatoid arthritis (RA) is a chronic auto inflammatory disorder that causes inflammation around the body and commonly presents with pain in the joints. It associated with morning stiffness and pain. leads to joint damage and deformity if untreated.
What is Symptoms of Rheumatoid arthritis ?
chronic pain, stiffness, tenderness, heat and swelling in the joints. RA can make it hard to move and perform daily activities.
What is Cause of Rheumatoid arthritis ?
Rheumatoid arthritis is an autoimmune condition, which means it’s caused by the immune system attacking healthy body tissue. However, it’s not yet known what triggers this.
Your immune system normally makes antibodies that attack bacteria and viruses, helping to fight infection.
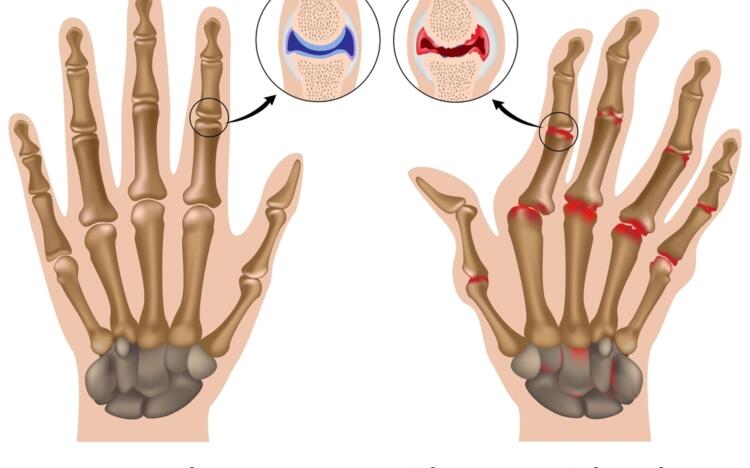
If you have rheumatoid arthritis, your immune system mistakenly sends antibodies to the lining of your joints, where they attack the tissue surrounding the joint.
This causes the thin layer of cells (synovium) covering your joints to become sore and inflamed, releasing chemicals that damage nearby:
- cartilage – the stretchy connective tissue between bones
- tendons – the tissue that connects bone to muscle
- ligaments – the tissue that connects bone and cartilage
If rheumatoid arthritis is not treated, these chemicals gradually cause the joint to lose its shape and alignment. Eventually, it can destroy the joint completely.
Various theories of why the immune system attacks the joints have been suggested, such as an infection being a trigger, but none of these theories has been proven.
What is Risk Factors of Rheumatoid arthritis ?
There are several things that may increase your risk of developing rheumatoid arthritis, including:
- Biological family history
- Hormones
- Sex
- obesity
- Smoking – Smoking increase a person’s risk of rheumatoid arthritis than men.
What is Diagnosis of Rheumatoid arthritis ?
The blood tests look for inflammation and blood proteins (antibodies) that are signs of rheumatoid arthritis. These may include:
Medical history. The doctor will ask about joint symptoms (pain, tenderness, stiffness, difficulty moving), when they started, if they come and go, how severe they are, what actions make them better or worse and whether family members have RA or another autoimmune disease.
Physical examination. The doctor will look for joint tenderness, swelling, warmth and painful or limited movement, bumps under the skin or a low-grade fever.
Blood tests. The blood tests look for inflammation and blood proteins (antibodies) that are linked to RA:
Erythrocyte sedimentation rate (ESR, or “sed rate”) and C-reactive protein (CRP) levels are markers for inflammation. A high ESR or CRP combined with other clues to RA helps make the diagnosis.
Rheumatoid factor (RF) is an antibody found (eventually) in about 80 percent of people with RA. Antibodies to cyclic citrullinated peptide (CCP) are found in 60 to 70 percent of people with RA. However, they are also found in people without RA.
Imaging tests. RA can cause the ends of the bones within a joint to wear down (erosions). An X-ray, ultrasound, or MRI (magnetic resonance imaging) scan can look for erosions. But if they don’t show up on the first tests that could mean RA is in an early stage and hasn’t damaged bone yet. Imaging results can also show how well treatment is working.
What is Treatment Rheumatoid arthritis ?
The goals of RA treatment are to:
Stop inflammation or reduce it to the lowest possible level (put disease in remission).
Relieve symptoms.
Prevent joint and organ damage.
Improve function and overall well-being.
Reduce long-term complications.
Early, aggressive treatment to reduce or stop inflammation as quickly as possible.
Targeting remission or another goal (called “treat-to-target”) to work toward few or no signs or symptoms of active inflammation.
Tight control to keep inflammation at the lowest level possible.
1 DMARDs( Methotrexate)
2 Biologic Agents
3JAK inhibitors
4 NSAIDs
5 Steroids
6 physiotherapy and lifestyle changes
